Core Requirements
Capstone
Elective
3CU
n/a
3 CUs total
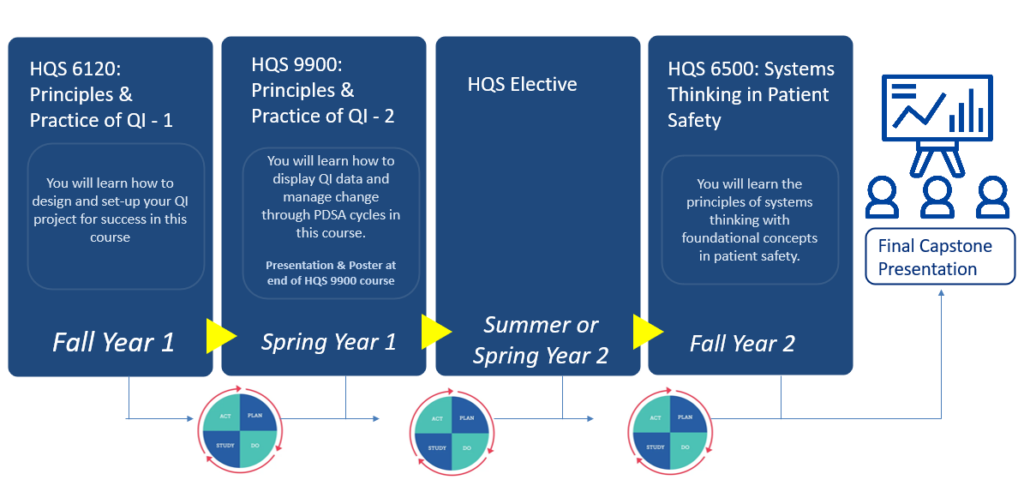
Healthcare delivery is complex and constantly changing. A primary mission of leading healthcare organizations is to advance the quality of patient care by striving to deliver care that is safe, effective, efficient, timely, cost effective, and patient-centered. The goal of this inter professional course is to provide students with a broad overview of the principles and tools of quality improvement and patient safety in health care while also guiding them through the steps of developing a quality improvement project. It will provide a foundation for students or practicing clinicians who are interested in quality improvement and patient safety research, administration, or clinical applications. As part of this course, students will design and plan for a real quality improvement project in their area of interest within healthcare using the methods and tools taught in the course.
Taught by:
Jennifer S. Myers, MD and Heather Greysen, PhD, CRNP
Course usually offered in fall term
Also Offered As: NURS 612
Activity: Lecture
1.0 Course Unit
Building on prior coursework that provided a broad overview of the principles and tools of quality improvement in healthcare, this course will provide students with in-depth knowledge of quality improvement (QI) methods, tools, and measures with a strong focus on focus on implementation and sustainment of change. Additional content includes change management, measuring for improvement, sustainment of interventions, QI scholarship, and professional development. Using assigned readings, class lectures, discussion, experiential learning, and in-class exercises, students will apply the methods and tools taught in this course to conduct a quality improvement intervention in their healthcare organization. Students will incorporate concepts related to knowledge-based care, patient-centered care and systems-minded care when developing process improvement changes. Additionally, students will reflect on knowledge gained from the application of these process improvement tools and the challenges of implementing changes in a healthcare organization.
Taught by:
Jessica Hart, MD, MHQS and Patricia Macolino, MSN, RN, CSSBB
Course usually offered in spring term
Activity: Hybrid
1.0 Course Unit
This blended online/in-classroom graduate level course integrates principles of systems thinking with foundational concepts in patient safety. Utilizing complexity theories, students assess healthcare practices and identify factors that contribute to medical errors and impact patient safety. Using a clinical microsystem framework, learners assess a potential patient safety issue and create preventive systems. Lessons learned from the science of safety are utilized in developing strategies to enhance safe system redesign. Core competencies for all healthcare professionals are emphasized, content is applicable for all healthcare providers including, but not limited to, nurses, pharmacists, physicians, social workers and healthcare administrators, and may be taken as an elective by non-majors.
Taught by: Susan Keim, PhD, MSN, MS, CRNP and Kathy Shaw, MD, MSCE
Course usually offered in spring term
Also Offered As: NURS 650
Activity: Lecture
1.0 Course Unit
The purpose of the quality improvement capstone is to provide a culminating experience in the program that requires the integration and application of knowledge attained in pre- and co-requisite coursework. The Capstone will build upon prior coursework that provided a broad overview of the principles and tools of quality improvement and patient safety in healthcare with a focus on implementation and sustainment of change. Students will apply this knowledge through completion of a mentored quality improvement project in a healthcare organization. In collaboration with faculty and health organization advisors, students will identify a quality improvement opportunity and use improvement methodology to describe the extent of the problem, analyze the current system, design tests of change (countermeasures), implement at least two plan-do-study-act cycles, and measure results. Students will also reflect on lessons learned and process of change.
Students will present their work in the spring semester.
This course provides a national perspective on the history and evolution of the US healthcare quality movement and the six components for high quality healthcare: safe, timely, effective, equitable, efficient, and patient-centered. Using a mix of local and national leaders in the field, the complexities of quality and the scientific basis for understanding the measurement of quality will be explored, including exposure to quality measures from a variety of organizations and measure comparison sites and the merging of quality outcomes with evolving reimbursement paradigms and models. The association between quality and safety and healthcare economics, regulation, accreditation, information technology, and population health will also be covered.
Taught by: David Horowitz, MD and Neha Patel, MD,MS
Course usually offered summer term only
Activity: Lecture
1.0 Course Unit
This intensive graduate institute applies core clinical informatics concepts in the context of quality improvement and patient safety initiatives. Content covered addresses foundational theories, frameworks, and policies of clinical informatics relevant to quality improvement and patient safety as well as practical application of informatics tools relevant to quality improvement efforts and local governance structure. Learners will be exposed to a variety of informatics leaders from across both the University of Pennsylvania Health System and Children’s Hospital of Philadelphia. The course is offered in both abbreviated (0.5 CU) and comprehensive (1.0 CU) versions. Those taking the comprehensive course will have exposure to material on advanced analytics strategies and hands-on data management. A hybrid structure of in-person days with one virtual day, and optional offers hours is intended to allow flexibility for learners while maximizing beneficial interactions and active participation between learner, instructors, and building the UPHS/CHOP informatics community.
Taught by: Srinath Adusumalli, MD, MSHP, MBMI and Leah Carr, MD
Course usually offered in summer term
0.5 Course Units OR 1.0 Course Units options
This course provides an overview of quantitative and qualitative methods for evaluating quality improvement and patient safety (QI/PS) efforts in healthcare. Through the use of assigned readings, discussion, and assignments, students will develop skills to critique evaluations of existing QI/PS projects and design a robust evaluation of a healthcare improvement initiative. Topics include the principles of good measurement, development of performance measures, intermediate and advanced concepts in statistical process control, and the research methods used in the evaluation of QI/PS interventions.
This class meets weekly both online and in person.
Taught by: April Taylor, MS, MHA, CPPS, CPHQ
Course usually offered in fall term
Activity: Lecture
1.0 Course Unit
This six-week course will help develop core skills for emerging leaders of safety and quality in healthcare systems. The course will include a combination of self-assessments, encounters with exemplary leaders, group exercises, individual activities and readings that will provide the participants with a range of experiences designed to further student’s own leadership journey.
Taught by: Daniel Hyman, MD, MMM
Course usually offered summer term only
1.0 Course Unit.
This course provides learners with the tools to address health and health care inequities using quality improvement methods. Learners will be able to explore the upstream causes of health and healthcare inequities including historical and current day practices routed in racism, sexism, classism, and queer-and-transphobia, among other practices of oppression. This course explores different methods for the purposes of using them in conjunction with quality improvement (QI) frameworks to ensure health equity as a positive outcome of QI efforts. Common QI frameworks and outcome measures will be reviewed with a focus on how to use them in health equity QI work. In addition, the course includes topics of leadership and change management in order to support successful collaborations resulting in health equity. Learners will apply these themes in a final project, engaging an example of an inequitable processes or care to design a QI project with the goal of improving health equity.
Taught by: Renee Betancourt, MD and Tyneshia Harris Howzell, MSHS, LSSGB
Course usually offered spring term only
Activity: Hybrid (Class meets twice monthly)
1.0 Course Unit
Copyright © 2024 The Trustees of the University of Pennsylvania